When the cure is worse
Canada’s so-called Indian hospitals were depressing places that segregated, abused and even experimented on aboriginal patients. Gary Geddes speaks to those who were there about their long and painful legacy
Gary Geddes
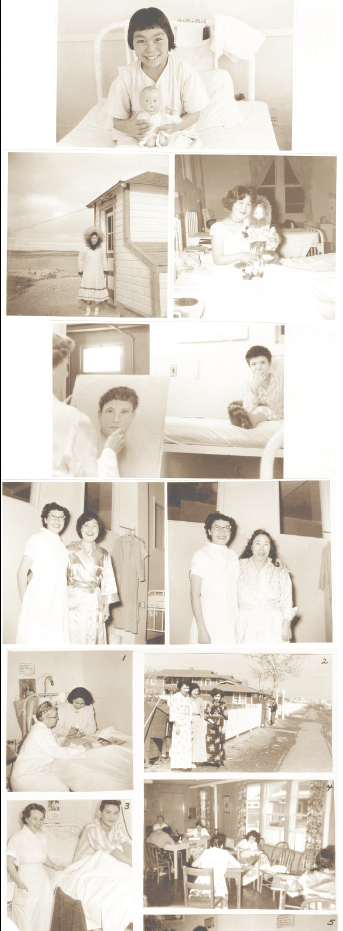
All photos courtesy Provincial Archives of Alberta
The first image: a small child in striped pyjamas, three years old, peering through the bars of a crib, directly into the lens of the camera. There’s intelligence in her eyes, but no indication of pleasure or recognition. Just a quiet, cautious curiosity. She’s holding a naked, hairless, rubber doll. Behind her, off-kilter on the wall, are two framed drawings, one of a kitten, the other of a girl hugging a rabbit. The scene is a ward in Edmonton’s Charles Camsell Indian Hospital. The year is 1960. The child is Linda McDonald, from the Liard First Nation in the Yukon, recently diagnosed with tuberculosis. The solitude and vulnerability emanating from the photograph are not surprising, given her age and the abruptness of her departure. “My earliest memory is of mom walking with me to the little lake we lived beside,” she tells me, more than five decades later. “She carried me in her arms and she was crying. That is all I remember of mom saying good-bye. I then recall being on a plane with someone.”
Arrival at Camsell was no less traumatic: “The bathroom seemed very large. A nurse all in white was taking my clothes off and making me stand in a shower. I think this was my first shower experience. I was crying and she said, ‘shut-up’ and banged my head against the wall of the shower. I remember the smell of the bathroom, the large bars of Ivory soap.” Another of McDonald’s memories of Camsell involves being awakened in the middle of the night by a siren, by shouting and people running, and not knowing what was happening. A head-count on the lawn revealed someone was missing. McDonald recalls a nurse using the scissors to cut the cloth bonds that tied her to the crib and carrying her out where the rest were gathered.
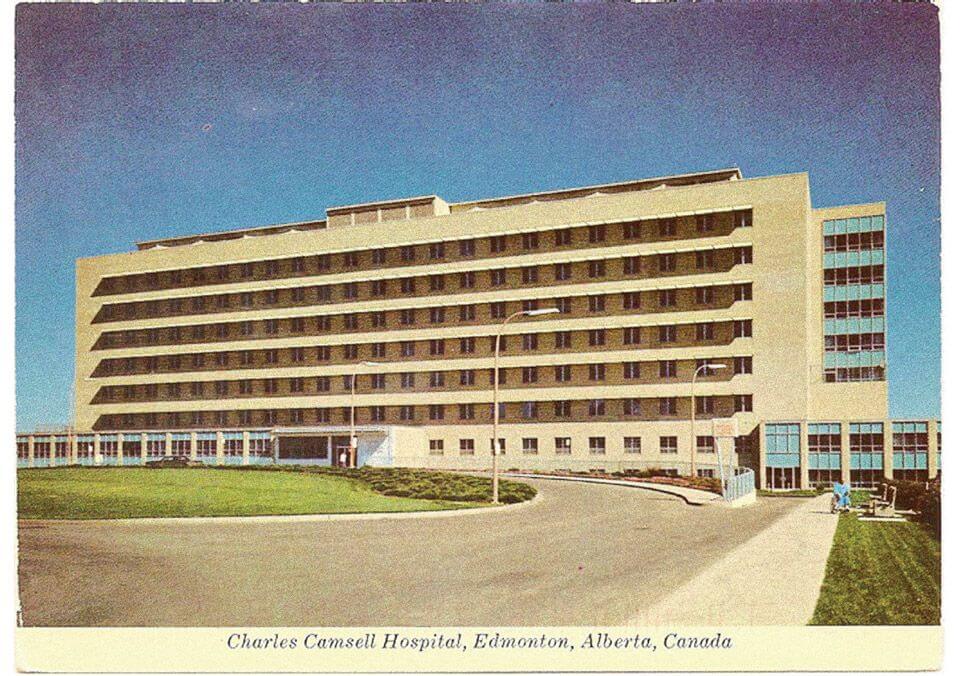
I first heard from her in response to a brochure I distributed at the hearings of the Truth and Reconciliation Commission (TRC) in Vancouver in September 2013. On the cover was an image of four small girls in dressing-gowns overlaid with the caption: “What Was Going on in Canada’s Indian Hospitals?” Inside, along with a photograph of Camsell, was a description of the link between the racially segregated hospitals for aboriginals and residential schools: the latter serving as farm-teams or recruiting grounds for the former, providing a constant clientele of guinea pigs for forced sterilization, gratuitous drug and surgical experiments, and electric shock treatment—a sure way to destroy the short-term memory of sexual abuse. “I went into the hospital
an Indian girl,” McDonald confides, “and came out a white girl.”
I met her a few months later in Whitehorse. At the time, she was just finishing a six month medical leave from teaching. The person I met was out-going, middle-aged, and very bright. We had a wonderful lunch together and she arranged for me to meet several of her friends who had also been patients at the Camsell. Without those emails and beautifully written memoirs, I would not have guessed there was anything troubling this charming and vivacious person, whose life had been so profoundly affected by her two solitary years peering through crib bars, wearing pyjamas that resembled striped prison garb, and who had returned home “spoiled and thinking our little cabin was dirty and smelled funny.”
Yet, her experience was not unique. Camsell was one of 22 segregated hospitals in Canada, created not so much to help the Indigenous population, as to keep them separate from the white community. Established on racist assumptions, it’s not surprising that these hospitals were poorly staffed and underfunded. While residential schools— with their death-rate of 40-60 percent—are now widely acknowledged as a horrible stage in a slow-motion genocide, the story of the socalled “Indian hospitals” has been largely ignored. And yet, their legacy continues in today’s health care system. Were it not for this ongoing racism and colonial legacy, for instance, Brian Sinclair, a 45-yearold Indigenous man and double-amputee, would not have died in his wheelchair in a Winnipeg emergency room in September 2008 after being left unattended for 34 hours with a kidney infection that could have been treated.
Speaking of the Camsell era, medical researcher and author of Healing Histories, Laurie Meijer Drees offers the understatement of the year when she informs us it’s clear that, in Canada, aboriginals “mattered less.”
Provincial Archives of Alberta
Systemic racism is no stranger to Canada. British Columbia, my home, not only spearheaded the evacuation of thousands of Japanese-Canadians during World War II, but also gave enthusiastic support to the Chinese Head-Tax and the refusal to allow the Komogatu Maru to dock in 1913 in Vancouver harbour, sending it back to Hong Kong with its cargo of Sikhs and their shattered dreams of immigration. B.C. was also quick to follow suit when its neighbour across the Rockies passed the Alberta Sterilization Act in 1929, both provinces paying doctors to perform involuntary surgical procedures, a disproportionate number of them done on Indigenous men, women and girls. The provinces were in tune with the federal government, which turned away the St. Louis and its shipload of Jews fleeing the Holocaust, because someone in the Ottawa bureaucracy thought one Jew too many.
Treaty 7, signed between the Crown and First Nations in Southern Alberta in 1877, came with no promise of medical assistance—not even the standard clause of a medicine chest, which had been included in earlier treaties. Neither did Treaty 8, which covered Northern Alberta, B.C. and part of the NWT. A secondary report by Indian Commissioner David Laird promised that “supplies of medicine would be put in the charge of persons selected by the Government at different points, and would be distributed free to those of the Indians who might require them.” Laird and his contemporaries assured aboriginal signatories that “the government would always be ready to avail itself of any opportunity of affording medical service,” although these promises were not written into the treaty itself. The federal government would pay little attention to the health of aboriginals for decades, eventually downloading the responsibility to the provinces.
Another former Camsell patient, Marilyn Murray-Allison, a Gwich’in woman from the NWT, contacted me to say that both she and her mother had been patients in the early 1950s. Age five-and-a-half, and in constant pain, she could neither sit nor stand. Together with her parents and her sister, she was flown to the hospital, where staff found tuberculosis in her lymph glands; her mother had it in her lung. “It was a very tragic time,” she says. “In a matter of a few hours, our family was separated.”
The separation anxiety, rather than the tuberculosis, almost killed her. Although in the same hospital, mutual contact between family members was disallowed on the assumption that it would be upsetting to both parent and child who were supposed to be immobile and resting. But separation in a strange place, where no one spoke her language, made it worse. “All I remember of those days,” says Murray-Allison, “was the hurt and sadness and crying for my mother and my family. I was dying of heartbreak, not being able to eat and biting my fingernails until they were bleeding.”
Eventually, staff realized she wasn’t improving and put her in a room next to her mother’s. Able to see her mother through a window in the wall that still separated them, she began to heal slowly. More than once, a kind nurse would wrap her frail body in a blanket and sneak her in to cuddle with her mother. Bedridden for so long, she forgot how to walk and had to learn all over again.
Such procedures do not speak well of either the medical knowledge or the psychological insight of doctors and nurses, whom we might expect to know something about the role of emotions in the healing process. In The Camsell Mosaic, a book put together by the hospital’s history committee, Dr. William Barclay acknowledges the severe limitations under which staff worked and the primitive measures taken to treat patients. He describes how, initially, no drugs were available for the treatment of tuberculosis, so total bed rest was prescribed, sometimes including surgical collapse of the lung and plaster casts to fixate the joints, most of these procedures applied in “blind faith.”
Among the many Camsell photos in Meijer Drees’ Healing Histories and in the federal government’s archives, there is one that touches me deeply. It shows 11 children, aged two or three, in white gowns arranged on benches by a nurse wearing a facemask. The two in the front row wear moccasins, another child is missing a shoe and a third is sucking her fingers. Collectively the photograph does not depict a single mood, such as fear or anguish or pleasure—though the children are anything but animated. Yet, knowing how children need the love and affection of parents—and how their health and immune systems can plummet without this special care—the photo sends a shiver down my spine. Many of those toddlers—if they even made it through their hospital ordeal— were not sent home, but shipped off immediately to residential schools, where their chances of survival were sometimes as low as 60 percent.
Relevant to the story of these segregated hospitals is Canada’s long-standing policy not only of ignoring aboriginal wellbeing, but also of deliberately starving Indigenous peoples to force them into white subservience. Many of the great chiefs, including Poundmaker and Big Bear, were brought to their knees as beggars, asking for handouts to save their people. The violence that prompted killings at Frog Lake in 1885 and helped spark the Riel rebellion in the prairies was precipitated by Canada’s high-handedness and failure to fulfil treaty promises, particularly the failure to provide food and medicine after the extermination of the buffalo. As Maureen Lux explains in Medicine That Walks: Disease, Medicine and Canadian Plains Native People, 1880-1940, the starvation of the tribes at Fort Walsh, “was a cynical and deliberate plan to press the government’s advantage and force the Cree from the area and allow the government a free hand in developing the prairie.”
It has taken more than 100 years to dismantle some of the myths about Canada’s Indigenous peoples, including the notion that they are more susceptible to disease than other races. Appalling conditions, rather, were to blame for the high rate of morbidity: hunger, malnutrition, being crammed into tiny reserves, and held captive in residential schools that were often a haven for diseases, sadists, and pedophiles. Continual neglect and abuse resulted in fatalities that, in earlier times, might have been avoided, or at least less widespread, when food, confidence, and solidarity were not in short supply. These exacting measures were approved at the highest level of government. Prime Minister John A. Macdonald made this clear in 1882 when he assured the House, “we cannot allow them to die for want of food,” then added that Commissioner Edgar Dewdney and the Indian agents, as they wer called at the time, “are doing all they can, by refusing food until the Indians are on the verge of starvation, to reduce the expense.”
When Dr. Peter Bryce, chief medical officer of the Department of Immigration, was sent out to study the conditions in prairie residential schools in 1907, he wrote a scathing report about what he witnessed, including overcrowding, malnutrition, and an appallingly high death rate. His report was shelved and his position eliminated. Fifteen years later he would publish the report himself under the title A National Crime. Duncan Campbell Scott, deputy superintendent of what was then called Indian Affairs, dismissed Bryce’s claims, saying in April 1910: “It is readily acknowledged that Indian children lose their natural resistance to illness by habitating so closely in these schools, and that they die at a much higher rate than in their villages. But this alone does not justify a change in the policy of this department, which is geared towards the final solution of our Indian Problem.” On another occasion he added: “It is only necessary to carry out some common sense reforms to remove the imputation that the department is careless of the interests of the children.”
Those promised reforms, of course, did not come. Lux tells us that Chief Long Lodge, whose people had been forcibly removed from Fort Walsh in the Cypress Hills of southern Saskatchewan and were sick from starvation, put the matter bluntly: “I want no government medicine. What I want is medicine that walks. Send three oxen to be killed and give fresh meat to my people and they will get better.” When the aboriginal population—albeit one that was devastated and drastically reduced in numbers—refused to disappear, residential schools and segregated hospitals were the next phase of the “final solution” that Indian Affairs (now Aboriginal Affairs and Northern Development Canada) set in motion.
Forced sterilizations and drug and surgical experiments happened in many segregated hospitals during the two decades following World War II. Teeth were often removed without freezing and experimental drugs were administered that caused serious harm, or proved fatal. The causes of death were often falsely reported to authorities and loved-ones were not contacted. Sexual abuse was not uncommon, as many testimonies at the hearings of the TRC confirm. One friend told me an orderly raped her at the Nanaimo Indian Hospital while her upper body was encased in an iron lung. Much of the fear that Indigenous people have of doctors and hospitals today derives from the horrendous experiences and racist attitudes encountered in these institutions.
Provincial Archives of Alberta
As I was putting these thoughts together in January 2014, Melinda Bullshields phoned me from her small flat on East 2nd Avenue in Vancouver’s East End to say she’d seen one of my brochures at the TRC. One of 11 siblings from the Blood Reserve in Alberta, about 30 kilometres from the U.S.-Canada border, she’d been a patient at the Camsell from age four to eight. Simply put, it ruined her life. Her voice was strong, urgent, articulate, informing me that being bedridden for so long made her knees small for her size, but she’d still managed to become an athlete. She saw many things at Camsell—every kind of abuse, “I remember the casts, little kids with hips and both legs in a body cast, just a small hole where they could pee,” she says. “At night, the orderlies would be doing things in those holes.”
Four years of hospitalization, followed by residential school, alienated her from family, some of whom she no longer recognized when she returned to the reserve. “They groomed me for solitude,” she says. “I coped with the abuse by dissociation, closing off the emotions, being elsewhere when nasty things happened to me.” This dismal situation continued even back home, where her sisters tormented her for being too English and where the worst abuses learned in residential school and the segregated hospital had become an epidemic.
When we met at a coffee shop on Commercial Drive in Vancouver, Bullshields brought her copy of The Camsell Mosiac to show me her photo on page 211, front row, third from the left—one of 10 tiny, costumed girls, part of the Counterpane Players, wearing a frilly, conical cap, her only photo of herself from that period, a light moment in an otherwise dark period. “I hate both sides,” she says, “so where does that leave me?”
Indeed, where does this leave all of us? As individuals and as a nation, we have a responsibility to rewrite the national narrative, acknowledging our failure to honour the promises and partnership
implied in the treaties and to build a better, stronger, healthier future. We can start by making the records of all 22 segregated hospitals available. Canadians need to know what really happened in these hospitals—the sterilizations and the nutritional, drug, and surgical experiments. We also need to find out what was going on in that special day school on the Goodfish Lake reserve in Alberta where, from 1959–1963, 38 Cree children were isolated, taught nothing, allowed to watch TV all day, and subjected to excessive doses of polio vaccines, known even then to be contaminated with a carcinogen called SV40—a virus originating in the kidneys of the rhesus monkey used as a culture for growing the vaccines.
Camsell would be a good, symbolic place to jump-start the reconciliation and healing process. After serving as a general hospital for the entire population from 1967–1996, it was abandoned because of asbestos contamination. It remained empty for decades, grew increasingly decrepit, and only made the news periodically, when vandals started fires or the building figured in the internet’s latest ghost watch.There was enlightened talk of renovating and turning it into housing for Edmonton’s homeless and low-income population, a large number of whom are First Nations individuals, but the locals objected. Instead, the city sold the building to a developer, who promised to turn it into condos for seniors and yuppies. Now that the asbestos has been removed, the city council could intervene to realize that earlier dream.
Harold Cardinal wrote many years ago in The Unjust Society that equality of health or education services is not enough: “We aren’t starting on equal grounds. Equality of services doesn’t mean a thing to people who are so far behind they can’t even see the starting line. It just means we would remain that far behind. That’s not good enough. We want to catch up. Then we can talk equality.” Cardinal, who was born in High Prairie, Alta. and grew up on the Sucker Creek Cree Reserve, wrote those words in 1969. Some 46 years later, we have still not taken them to heart.
Between 1946-1966, nearly 97 Indigenous patients who did not survive Camsell, including 13 infants, were buried in the cemetery on the grounds of the former Edmonton Indian Residential School, located in nearby St. Albert. Their names are inscribed on marble slabs on four sides of a monument made of round stones set in concrete. On the top of the six-foot-high structure, between the stones, mourners have deposited tiny plastic toys and a small skipping rope. When I visit the site in late April 2015, a cold wind has blown a tiny, black, plastic car onto the paved surface. I pick it up and place it back on top of the monument, wondering about those who left it here.
Before departing, I drive a few hundred metres to the new Poundmaker drug and alcohol addiction centre that now occupies the grounds of the former residential school. A stand of poplars in the distance is festooned with long, brightly coloured cloths. I ask a woman outside having a smoke what they signify.
“They’re prayer flags,” she tells me. “When the wind blows, they flutter and the pain is carried off by the breeze.
GARY GEDDES has written and edited more than 45 books and won a dozen national and international literary awards. His most recent works are Swimming Ginger, Drink the Bitter Root, and What Does A House Want? He lives on Thetis Island, B.C.